By Dr. Howard Dananberg
Hallux limitus is a very common and painful condition which affects the 1st metatarsophalangeal joint. The prevailing view of this entity is that it is a degenerative process that proceeds over time to progressive loss of motion and increase in pain with associated walking disability. This article will examine this not in the classic sense of a degenerative process, but rather one of repetitive daily trauma, with the inflammation and bone proliferation being part of a daily “repair” process. Interestingly, it relates in large part to chronic muscular inhibition of the peroneus longus. This muscular dysfunction results in a dorsiflexed first ray unable to permit normal functional plantarflexion/eversion, causing jamming of the joint, which ultimately leads to its classic enlarged, stiffened appearance.
Inhibition is a well-documented neuromuscular action. Inhibition and its converse, facilitation, are normal muscular actions mediated by the central nervous system. As their names imply, facilitation acts as a stronger response, and inhibition a weaker one. This becomes a very useful mechanism for smoothing and controlling joint movements. For instance, antagonistic muscles of the arm (biceps and triceps) are both oppositely facilitated and inhibited to manage lifting weights in a biceps curl exercise.
When the biceps contracts, the weight is not violently moved as the inhibited triceps mediates the response of the facilitated biceps. This effectively creates a modulation to muscular control of joint movements. If the triceps were not inhibited, it would exert an overwhelming opposing force so as to prevent the biceps from flexing the elbow. If not on at all, it would create an unopposed contraction of the biceps, with the weight striking the lifter in the face!
All opposing muscles seem to create balanced motions via this mechanism. When muscles, however, become negatively impacted by what appear to be very subtle injuries, it can result in a chronically weakened state. And when related to a dysfunctional joint, it becomes known as an arthrogenic inhibition. Since neurologic signaling continues, albeit incorrectly, there is no obvious atrophy as seen when total motor control is lost. This inhibited state can ultimately lead to pain at the joints about which these particular muscles function, yet be hidden as an etiologic factor.
Although documented, the reason why muscles become chronically inhibited is not well understood. In the case of the peroneus longus, it appears that its inhibitory status is dependent on a subtle but critical translation motion of the fibula. With ankle joint dorsiflexion, the fibula is not fixed in place, but rather glides cranially and laterally with respect to the tibia, and then reverses with plantarflexion. This translation is easily palpated at the fibula head and serves many purposes. At the ankle joint level, this gliding widens the joint space and permits the wider anterior talar dome to easily fit into the mortise, allowing unimpeded dorsiflexion.
At the fibula head level, it relieves tension from the lateral hamstring (biceps femoris), which inserts directly into the fibula head. The biceps tendon was always believed to originate directly from the ischial tuberosity. However, Andre Vleeming, PhD from Belgium has shown it to actually arise from the fibers of the sacrotuberous ligament. The lateral hamstring is therefore anatomically connected to the sacrum (base of the spine). As the fibula translates, it allows for a reduction in hamstring tension, a requirement for the sacral motion known as nutation. Nutation is known to stabilize the base of the lumbar spine in a similar fashion to the way subtalar joint supination acts to stabilize the foot. Failure of nutation to occur (counter-nutation) can lead to chronic lumbar instability, similar to the way a maximally pronated subtalar joint leads to an unstable foot.
Restriction in fibula motion is quite common but rarely recognized. It is usually caused by some type of trauma, such as an inversion type foot/ankle sprain. This can range from severe to very mild. The pain need not be immediate, nor even recognized as an injury. Without probing on history-taking, there is often no relevant information gleaned unless the examiner has a high sense of suspicion. Symptoms of the 1st MTP joint are not necessarily immediate and often begin with a gradual sense of pain, dysfunction in the joint, or swelling with an associated complaint of shoe tightness across the forefoot. They progress over time depending on activity level.
In athletes, it is not uncommon to be diagnosed with turf toe in the weeks or months following an ankle sprain. These same athletes further complain of a fear of a repeat ankle rollover as it seems unstable laterally. With the posterior tibial muscle being unopposed by what should be a normally facilitated peroneal group, a chronic bias towards inversion develops as a consequence. This common “inverted” finding further points to the underlying peroneal inhibition as the primary etiology.
Manual Manipulation
Manual manipulation of joints predates Hippocrates. Records in Egyptian literature describing various mobilization techniques existed by 1500 BC. Manipulation of the ankle has been shown to be a safe and highly effective method of care which both returns fibula range of motion and restores peroneal facilitation (A video of this is available at https://www.youtube.com/watch?v=mrSQiQrAb5E).
Even in states of equinus, manipulation can offer a method of care by creating a change in range of motion of the ankle in addition to positive-ly altering the muscular inhibition/ facilitation neurology. Coupled with ankle manipulation, cuboid manipulation can also add significantly as the mobility of this bone is essential for normal peroneal function.
The exam begins with careful assessment of ankle joint dorsiflexion with the knee fully extended. During this initial phase of testing, the examiner can place one hand on the knee while the other positions the foot to as-sess range of motion. Should the knee flex as the patient attempts to dorsiflex the ankle, it is a sign of marked motion restriction at the ankle. By holding the knee fully extended, the limits of dorsiflexion can be truly assessed.
The next phase is to palpate the fibula head while the ankle is being dorsiflexed. A fibula head which can be felt sliding under the palpatory finger generally indicates normal fibula translation. Sometimes, comparisons to the opposite side help to determine the extent of the motion restriction.
When assessing the calcaneal-cuboid articulation, the simplest way to evaluate lateral column (4th and 5th rays) is to evaluate dorsal excursion while the rearfoot complex is held with the opposite hand. Failure to have unrestricted dorsal range of motion is a sign of calcaneal cuboid restriction(a video on manipulations of the cuboid is available at https://www.youtube.com/watch?v=Ryl8WqEOSJY .
Examinations of this 1st MTP joint rarely include muscle strength testing of the peroneus longus. While simple and relatively easy to perform, without strength identification of this as a potential etiology, it is overlooked and therefore not included in a differential diagnosis. This actually holds true for not only hallux limitus, but other painful conditions of the 1st MTP joint, including turf toe, sesamoiditis or even hallux valgus.
The technique of examination for peroneal strength involves its ability to act eccentrically, i.e., resisting dorsiflexion and inversion of the 1st ray. The examiner sits at the foot end of the exam table. The affected heel is rested on the end of the table, allowing for plantarflexion of the foot. One hand of the examiner is then placed on the lateral side of the foot, while the opposite hand is positioned over the medial malleolus for stability. The patient then maximally everts and plantarflexes the foot while the examiner tries to invert the foot. Lack of effective strong resistance to this maneuver is a positive test for peroneal inhibition (a video on this testing process is available at https://www.youtube.com/watch?v=AEe7SaSeCX8 )
The 1st MTP joint is a complex structure. It functions not as a simple hinge, but rather as a hinge glide combination to permit the appropriate dorsiflexion motion when this joint is under the peak load during the gait cycle. It uses the sesamoid apparatus to facilitate a plantarflexory motion designed to keep the 1st metatarsal head away from the base of the proximal phalanx. It is important to note that the hallux, once in ground contact, NO LONGER MOVES UNTIL TOE-OFF. It is the remainder of the foot and body that passes over the fixed hallux. Restriction in normal dorsiflexion becomes not just traumatic to the MTP joint, but to the more proximal structures as well, as it is their motion which is impeded.
Dorsiflexion of the 1st MTP joint is in large part permitted by the action imparted to the 1st metatarsal by the peroneus longus. It originates from the superior aspect of the fibula head, coursing laterally down the leg and then turning inferior to the lateral malleolus. It then runs medially under the peroneal groove on the plantar side of the cuboid, inserting into the base of the 1st metatarsal cuneiform joint.
In open kinetic chain, it would plantarflex and evert the 1st metatarsal head, but in closed kinetic chain, it actually resists the dorsiflexion inversion moment imparted to the 1st ray from ground reactive force. Therefore, failure of normal muscular activity would result in a dorsiflexed, inverted 1st ray. When the 1st ray becomes chronically adapted to this circumstance, jamming occurs at the MTP joint with each step.
In some cases, further compensation occurs, such as forefoot inversion, creating an avoidance response to this functionally inhibited joint function. Without avoidance, pain in the 1st MTP joint can develop, and the joint become further damaged via the thousands of step cycles taken on a daily basis. And each day this occurs, the body will attempt to repair this site via a perpetual inflammatory response to injury. Reversing this process involves a several-part treatment process.
Much of the current treatment philosophy of hallux limitus involves the concept that it hurts to move, so motion must be limited. Treatment therefore logically follows the thought process utilizing rigid soled shoes, steel plates, Morton Extension on orthotics, etc. This eventually becomes a self-fulfilling prophecy; limiting motion will only result in limited to no motion. The approach advocated in this paper looks at the pain of hallux limitus as being related to this joint not moving at the time when the motion is in the highest demand. Using joint manipulation to both increase motion and facilitate muscular action combined with orthotic prescriptions which enhance motion vs. restricting, it becomes an alternative method of care. There may be a short period of mild increase in symptoms as motion begins to be re-established, but this often resolves rapidly as gait style positively changes. Anti-inflammatory measures such as NSAIDs and/or ice can help in getting past this relatively minor hurdle. The only true contraindications to manipulation involve inflammatory disease, such as rheumatoid or psoriatic arthritis. Manipulation should NOT be performed in the presence of these or other inflammatory disorders.
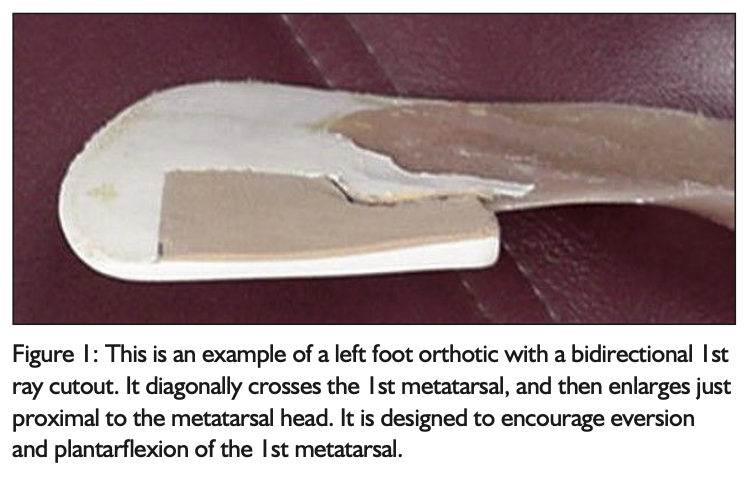
Orthotic management of hallux limitus also becomes a critical component in long-term care. Rather than using standard design prescriptions, an alternative approach is necessary. The use of 1st ray cut-outs becomes essential to permit timely 1st metatarsal head plantarflexion once the peroneals have become facilitated. There are several cutout designs which are highly effective in improving motion at this joint. These include the standard, bi-directional and long cutouts. The most interesting is the bi-directional. It uses a more acute cut along the shaft of the 1st metatarsal, and then a wider cut just proximal to the metatarsal head. This induces an eversion-type rotation to the metatarsal head, improving the release effect on the 1st MTP joint (Figure 1).
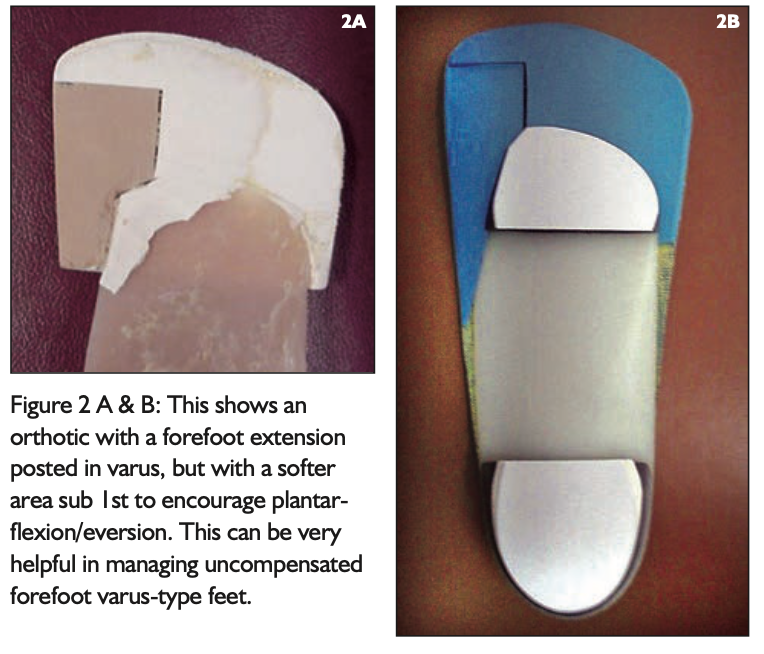
In some cases, the 1st ray has become so dorsiflexed that the foot appears with a marked inverted alignment such that it is unable to pronate and reach the support surface. Termed an uncompensated forefoot varus, it has been a very difficult type of foot to manage. Using the same principles as outlined in this article, an orthotic can be constructed that uses a forefoot varus post with extension, yet has a cut-out and softer material under the 1st metatarsal head. This can effectively bring the ground up to the foot, but also permits plantarflexion of the ray. In this manner, hallux dorsiflexion is permitted, but in a limited fashion (Figures 2A and 2B).
Most active patients dislike the notion of waiting until a problem is bad enough to ultimately have surgery. Conservative care options do exist and can improve the quality of life as well as long-term outcomes for specific types of disorders. A careful and thoughtful examination along with a treatment tool chest filled with various options for care are much appreciated by a patient population that desires answers rather than prolonged, painful waiting until surgery.
References
- Dananberg, Howard J, Philips AJ, Blaakman H. “A Rational Approach to the Nonsurgical Treatment of Hallux Limitus” in Advances in Podiatric Medicine and Surgery II, ed. Stephen J. Kominsky, DPM, Mosby; May 1996.
- Dananberg, HJ, Shearstone, J, Guiliano, M “Manipulation Method for the Treatment of Ankle Equinus, “ Journal of the American Podiatric Medical Association, 90:8 September, 2000 pp 385–389
- Dananberg, Howard J. “Gait Style as an Etiology to Chronic Postural Pain, Part I. Functional Hallux Limitus” in Journal of the American Podiatric Medical Association; August 1993.
- Dananberg, Howard J. “Gait Style as an Etiology to Chronic Postural Pain, Part II. The Postural Compensatory Process” in Journal of the American Podiatric Medical Association; November 1993.
Dr. Howard Dananberg practiced podiatric medicine in New Hampshire from 1976-2012. He is a contributing editor to JAPMA and a consultant to Vasyli Medical. He is the past winner of the Scholl’s Award for Outstanding Clinical Paper published in JAPMA, as well as being Inventor of the Week in the Lemelson-MIT Program for his creation of Insolia, a product which balances weight in higher heeled footwear for women, making them far more comfortable to wear.

